by owner-admin
Share

Achilles Tendinopathy: Education and Treatment
Achilles Tendinopathy: Education and Treatment
Imagine you’ve been grappling with relentless Achilles tendon pain, preventing you from running or playing on the court. Your doctor labels it as the usual Achilles tendinitis, prescribing the standard pain relief treatment of ice packs, anti-inflammatory medication, and rest. But as time ticks on, you’re still left with persistent pain, and you’re left wondering what other treatment options are available. Here’s the twist — your diagnosis and the prescribed treatment plan might not be hitting the mark. Contrary to the catchy term ‘Achilles tendinitis,’ which hints at inflammation as the main culprit, your discomfort might have a broader story to tell, known as ‘Achilles tendinopathy.’ This term ditches the inflammation focus and embraces a wider range of tendon issues, including degenerative changes in the tendon, which calls for a different treatment approach. In this article, we’re lifting the curtain on these terms, helping you grasp the essence of Achilles tendinopathy management, and giving you the tools to guide your journey towards effective recovery and rehabilitation.
Achilles tendinopathy is a common lower leg issue that affects both athletes and sedentary people. Historically this condition can cause long-lasting discomfort and frustration. In this article, we’ll explain what Achilles tendinopathy is and offer effective ways to manage it.
What Is the Achilles Tendon?
The Achilles tendon is a remarkable part of the lower leg. It starts from the calf muscles in your lower leg and foot, including the gastrocnemius and Soleus. These muscles are crucial for walking and running. The Achilles tendon is the body’s largest and strongest tendon, can handle up to 12 times your body weight when you run. (Source: Komi PV, Fukashiro S, Järvinen M. Biomechanical loading of Achilles tendon during normal locomotion. Clin Sports Med. 1992;11:521-531)
gastrocnemius and Soleus. These muscles are crucial for walking and running. The Achilles tendon is the body’s largest and strongest tendon, can handle up to 12 times your body weight when you run. (Source: Komi PV, Fukashiro S, Järvinen M. Biomechanical loading of Achilles tendon during normal locomotion. Clin Sports Med. 1992;11:521-531)
The Achilles is like a big rubber band that connects your foot to your lower leg. It acts as an elastic power source. When your foot hits the ground, the Achilles must stay firm, like a spring, to provide stability for your calf muscles to push you forward. For this to work well, the Achilles needs a solid “truss” (the foot) to attach to. Without a stable foot, the Achilles can experience abnormal stress, leading to strain and eventually tendinopathy.
Overloading the tendon -like when someone starts running for exercise and increases their distance or speed too quickly, can strain it. Tendons are designed to stretch and contract throughout the day, storing and releasing energy. However, they don’t handle twisting or torquing well while doing so. This happens when the front and rear of the foot are unstable and twist against each other.
The lack of foot control isn’t solely the foot’s fault. Issues in the lower back, hips, and knees can contribute to poor foot stability. A 2011 study by Munteneau et al found that individuals with Achilles tendinopathy often have delayed muscle activation in the lower leg, improper timing of hip muscle contractions, and reduced knee bending upon foot impact. All these problems add up, making the foot unstable for efficient movement. Athletes can develop it due to excessive training, while less active people might experience it due to weak calf and upper leg muscles. Other factors that increase the risk include hill running, speed work, poor recovery, limited ankle mobility, and muscular imbalance/ weakness.
Considering the stress the Achilles tendon endures during daily activities and sports, it’s no wonder this injury is common. A study in 2021 by DeVos et al. revealed that 2-3 people out of 1000 experience Achilles tendon symptoms. Another study by Kujala et al. found that runners have a 52% chance of encountering an Achilles injury in their lifetime with middle-aged male distance runners being more susceptible.
Types of Achilles Tendinopathy
There are two main types of Achilles tendinopathy, categorized based on the location of symptoms within the tendon: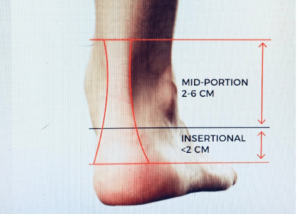
Mid-portion: Pain is localized 2-7cm above the Achilles tendon’s connection to the heel bone.
Insertional: Pain is localized where the tendon attaches to the heel bone
Recognizing Achilles Tendinopathy Symptoms:
Pain and stiffness when getting out of bed in the morning.
Pain that eases as you move around.
Pain when squeezing the tendon (mid-portion) or pressing on the heel bone (insertional).
Pain during activities like running, hopping, or jumping.
Reduced strength, endurance, and performance.
Swelling and thickening of the tendon at the painful site.
Effective Treatments for Achilles Tendinopathy
There are various treatment options for Achilles tendinopathy, but not all are equally effective. It’s important to know that tendinopathies take time to heal, and patience is key. You MUST temporarily stop activities that worsen the condition, such as running, jumping, or hopping. Use a heel lift or shoes with thicker heels (e.g., Hoka) for added support.
There’s no quick fix, but increasing research suggests that exercise is a powerful tool for managing Achilles tendinopathy but
research indicates that therapeutic exercise is one of the most effective treatments for overcoming Achilles tendinopathy. Exercise has strong evidence to support its role in optimal management and should be the primary treatment for at least three months before considering other options.
Additional treatments for Achilles tendinopathy include Platelet-Rich Plasma (PRP) injections, corticosteroids, non-steroidal anti-inflammatory drugs (NSAIDs), sclerosing injections, and shockwave therapy. However, a study in 2012 by Sussmilch et al. showed that none of these treatments, when used alone, were as effective as exercise therapy.
Best Exercises for Achilles Tendinopathy
While it’s natural to want to rest when something hurts, tendons actually benefit from being loaded and gradually worked. Extended rest can weaken the tendon and increase the risk of further injury. When it comes to Achilles tendon exercises, it’s okay to feel mild discomfort, rating it between 0 (no pain) and 4/10 (mild pain) on a pain scale.
However, it’s crucial to monitor your symptoms for 24 hours after exercising. If you experience pain greater than 4/10 and increased stiffness, you may have pushed too hard. Don’t worry! This just means your previous workout was a bit excessive. Instead of quitting, simply decrease the repetitions or sets in your next session. Start with Phase 1 and call me for an assessment and guidance through the next phases of exercise progression
Phase 1: Isometric Exercises
Isometric exercises are an excellent way to start strengthening an irritated Achilles tendon. These exercises help manage pain while gradually loading the tendon.
Standing Calf Raise Holds:
5-10 repetitions, hold for 10-30 seconds
Rest for 30 seconds between each repetition
Perform every other day
Wall Sit with Elevated Heel:
Keep knees at a 45-degree angle with your back supported against the wall
5-10 repetitions, hold for 10-30 seconds
Rest for 30 seconds between each repetition
If you’re frustrated with missing your runs and tired of letting your tennis partner know you cant make the match, AGAIN because your Achilles is on fire, don’t wait any longer. Take the first step to getting to back to the active lifestyle you desire, by taking advantage of our Discovery Session! It’s a Free 20 minute call to determine if PT is the right solution for you.
In Health,
Kim Mazik, MSPT,CEAC
EmPower Concierge Physical Therapy
208-309-0281
[email protected]



